AHIMA Survey on Patient Matching Illustrates HIM Burdens, Frustrations

The following post was submitted by Brad Marshall, Enterprise Development Consultant with RightPatient®
AHIMA Sheds Light on Patient Matching Problems in Healthcare
The American Health Information Management Society (AHIMA) released details of a survey yesterday that revealed over half of Health Information Management (HIM) professionals still spend a significant amount of time reconciling duplicate medical records at their respective healthcare facilities. The survey went on to reveal some very interesting statistics on patient matching and linking patient records, illustrating the burden that duplicate medical records have not only on HIM staff, but the dangers care providers face who increasingly rely on access to accurate, holistic patient data to provide safe, quality care. One particular stat that jumped out at us was:
“…less than half (47 percent) of respondents state they have a quality assurance step in their registration or post registration process, and face a lack of resources to adequately correct duplicates.”

A recent survey of HIM professionals by AHIMA illustrates the problems that duplicate medical records have on accurate patient matching in healthcare.
This is an area of particular concern due to the fact that our research has shown that many healthcare facilities spend tens, sometimes hundreds of thousands of dollars per year reconciling duplicate medical records but very few have technology in place to prevent duplicates in the future. It’s encouraging that accurate patient matching in healthcare seems to finally be getting the attention it deserves, due to the digitization of the industry, the shift change from fee-for-service to a value based payment system and a burgeoning healthcare ecosystem laser focused on improving both individual outcomes and population health. AHIMA’s survey supports this assertion by stating:
“Accurate patient matching “underpins and enables the success of all strategic initiatives in healthcare…”
Equally concerning is the fact that less than half of HIM professionals surveyed have any type of patient registration quality assurance policy in place and only slightly over half of survey respondents could accurately say what their duplicate medical rate actually is. Not to mention the fact that HIM professionals spend entirely too much of their time reconciling duplicate medical records, with 73% reporting that they work duplicates “at a minimum of weekly.”
As more healthcare organizations and facilities begin to understand that accurate patient matching has a major impact on other downstream activities, it is encouraging that the issue is finally getting the attention it deserves helped in part by the efforts of AHIMA, and CHIME’s national patient identification challenge which is scheduled to kick off this month. It’s clear that the healthcare industry is slowly coming to the realization that many new initiatives borne from the HiTech Act and Meaningful Use (e.g. – population health, ACOs, health information exchanges, interoperability) don’t really have any hope to succeed in the absence of accurate patient identification.
Duplicate Reconciliation Unnecessary Burden on HIM?
Early last year, we wrote a blog post on How Accurate Patient Identification Impacts Health Information Management (HIM) which highlights the exorbitant amount of time HIM spends reconciling duplicates and the opportunity cost this brings. For example, time spent on duplicate clean up and reconciliation could instead be allocated to coding for reimbursement and preparing, indexing, and imaging all paper medical records – a critical component in the effort to capture and transfer as much health data as possible to a patient’s EHR.
The fact of the matter is that as health data integrity stewards and medical record gatekeepers, HIM professionals are better served spending their time ensuring proper and accurate reimbursement and medical record accuracy then reconciling duplicates which should have never been created in the first place. HIM staff perform one of if not the most critical functions in healthcare by ensuring health data integrity, especially in light of the increasing reliance of often disparate healthcare providers need to access a complete medical record that includes as much information as possible.
As we noted in the post last January:
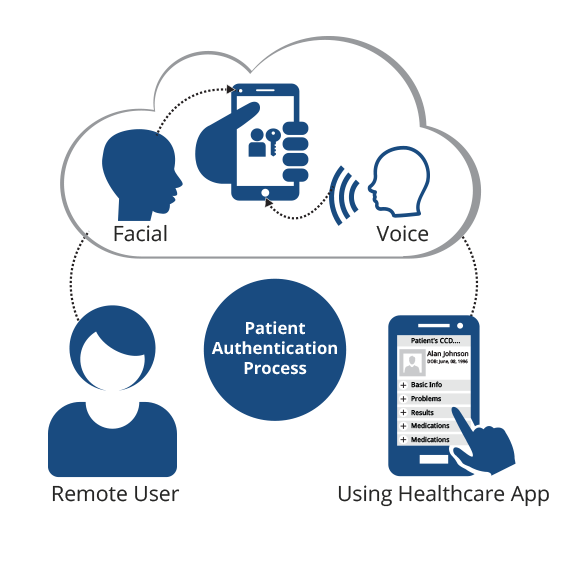
“…many hospitals have expanded responsibilities vis-à-vis Meaningful Use, EHR implementation, and meeting Affordable Care Act requirements, and it has become disadvantageous to continue devoting any time at all to duplicate medical record and overlay reconciliation. Biometric patient identification solutions open the door to re-allocation of HIM FTEs to more critical functions such as coding, reimbursement, and reporting. Simply put, implementing biometrics during patient registration is opening the door for HIM departments across the industry to provide a larger and more productive support role to meet the shifting sands of reimbursement and address the need to move towards quality vs. quantity of care.”
Conclusion
We could not have summed up the issue of duplicate medical record creation and reconciliation and inaccurate patient matching in healthcare more succinctly than this quote from AHIMA in the survey summary:
“Reliable and accurate calculation of the duplicate rate is foundational to developing trusted data, reducing potential patient safety risks and measuring return on investments for strategic healthcare initiatives.”
Trusted data. Isn’t this the backbone of the new healthcare paradigm? Certainly we can’t expect to achieve many of the purported advances in healthcare in the absence of clean, accurate health data. It’s time to eliminate duplicate medical records forever, and establish cohesive, quality assured patient matching in healthcare.
What are your biggest takeaways from the AHIMA report on accurate patient matching in healthcare?
 Brad Marshall is an Enterprise Development Consultant with RightPatient®. With several years of experience implementing both large and small scale biometric patient identification projects in healthcare, Brad works closely with key hospital executives and front line staff to ensure project success.
Brad Marshall is an Enterprise Development Consultant with RightPatient®. With several years of experience implementing both large and small scale biometric patient identification projects in healthcare, Brad works closely with key hospital executives and front line staff to ensure project success.