Patient Identification Errors in Hospitals Should be Eliminated Now Instead of Waiting for a UPI

Patient identification errors have been haunting the US healthcare system for decades now. In fact, the lack of effective patient identity management within the majority of hospitals and health systems is quite well-known as it is prevalent. Otherwise, groups would not have formed every year to appeal to Congress to finally approve a state-funded unique patient identifier (UPI). However, the coronavirus pandemic has been wreaking havoc across the US, which is why accurate patient identification is needed more than ever. But should they still wait for Congress for a UPI, or is there a way to eliminate patient identification errors in hospitals now? The short answer to the latter is yes – RightPatient. Let’s dive deep into the issues caused by patient misidentification, what the healthcare industry is doing about it, and how leading providers are solving it.

Issues caused by patient misidentification
Patient misidentification has always caused a plethora of problems – for patients, healthcare providers, insurance companies – basically anyone involved with patient care. However, the pandemic has deemed the elimination of patient identification errors in hospitals more necessary than ever, so that patients can get faster, more accurate care, leading to improved health outcomes. So, what are the issues caused by patient identification errors?
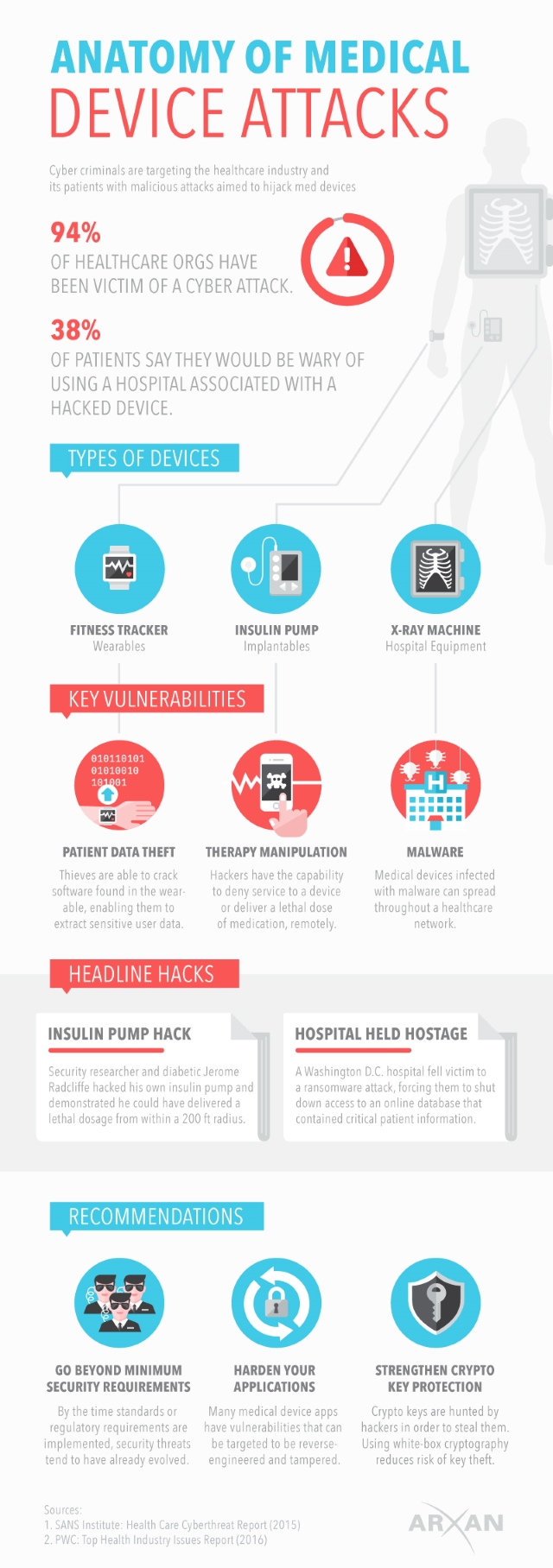
The lack of accurate patient identification can create duplicate records or overlays (merged medical records of the same or different patients), causing a ripple effect and hampering patient safety by generating inaccurate patient information. For example, a patient with a common name comes into a provider’s facility, and without a robust patient identification platform, it will be quite difficult for the EHR user to determine the correct medical record for the patient. Thus, the healthcare official will either painstakingly search for the correct record, which is quite time-consuming, or else an entirely new record will be created, leading to just another duplicate record among the several existing ones. Duplicate records create patient safety issues – patients will be treated based on an incomplete or inaccurate medical history. For providers, the financial cost of duplicates can be up to $40 million, according to AHIMA.

Patient misidentification can also cause denied claims, which have a severe impact on the financials of hospitals and health systems. Suppose a patient is misidentified by the provider using an obsolete patient identification system. While the patient at the facility will be receiving the care, someone else will be charged inadvertently for the services as a result of patient identification errors. However, the medical record holder can simply let the authorities know that someone else had used the healthcare services, and thus, he/she will not be charged – leading to a case of claim denial. Denied claims can cost up to $4.9 million on average for any given healthcare provider.
Even during this ongoing and unprecedented health crisis, patient misidentification is quite common. It occurs because there is no proper way to match patients to their electronic health records (EHRs) within those providers’ facilities, and it leads to patient safety issues as well as reduced quality of care. Other issues patient misidentification causes are incorrect treatments, medications, and lab test results – hampering patient outcomes significantly. Given the current scenario of the healthcare system, these issues should be minimized as much as possible – something that RightPatient can help hospitals with.
What is the healthcare industry doing about it?
During a virtual briefing, the CEO of AHIMA, Wylecia Wiggs Harris, stated that COVID-19 shows how important accurate data is and why patient misidentification issues must be solved as soon as possible.
 Likewise, other experts have been making similar statements. For instance, even COVID-19 test results were affected by patient identification errors. After the results came in, it was quite difficult to identify and search for the patients, as no accurate patient identity management system existed within the facilities.
Likewise, other experts have been making similar statements. For instance, even COVID-19 test results were affected by patient identification errors. After the results came in, it was quite difficult to identify and search for the patients, as no accurate patient identity management system existed within the facilities.
Thus, healthcare leaders across the states are coming together to once again to ask Congress to lift the archaic ban on a state-funded UPI. However, if the past has anything to teach, it is the fact that the ban has been in effect for decades now. Lawmakers and officials placed the ban citing privacy concerns regarding a UPI, and it is quite unlikely that they will budge now.
Instead, many leading providers have taken it upon themselves to eliminate patient identification issues within their premises themselves. How are they doing that?
Eliminate patient identification errors in hospitals now
Forward-thinking providers did not rely on Congress to remove the ban, which might not happen anytime soon, admittedly. Instead, they deployed RightPatient – the leading photo-based biometric patient identification platform.
It locks the medical records of the patients with their photos – a returning patient looks at the camera, allowing the platform to identify the correct medical record within seconds. It is completely hygienic and ideal for the current crisis.
Our platform has been successfully reducing patient identification errors in hospitals and health systems. RightPatient ensures accurate patient identification, reduces claim denials, avoids duplicate medical records, and even prevents medical identity theft – improving patient safety and quality of care in the process.
Contact us now and ensure accurate patient identification at your facilities to stay ahead of the curve.





 RightPatient is the healthcare industry’s leading photo-based biometric
RightPatient is the healthcare industry’s leading photo-based biometric