Denied Medical Claims Are Costly but Preventable with Patient Identification

The U.S. healthcare system is no stranger to problems, unfortunately. In fact, it has been plagued by a plethora of issues for several years. While some of the problems are definitely solvable, external issues alongside other factors cause the problems to continue. Some of the many problems are astronomical prices, the lack of price transparency, interoperability issues, the abundance of data breaches, medical identity theft, and patient safety issues. While we have covered some of these topics at one point or the other, let’s take a look at another crucial problem, denied medical claims, how they are problematic for everyone, and how positive patient identification can prevent them.
Denied medical claims are costly and cumbersome for everyone involved
Denied claims are not a recent problem within U.S. healthcare – most hospitals and health systems are quite familiar with them. One can safely say that denied medical claims are quite expensive – an average hospital can lose around $3.5 million due to them. However, denied claims not only affect hospitals but also insurers and patients, albeit in different ways – let’s see how.
Claim denials in a nutshell
In the U.S., healthcare is closely related to reimbursements from Medicare, Medicaid, and commercial insurers. Patients get health insurance, go to their healthcare provider, get treated, and that’s about it. However, a lot more goes on behind the scenes regarding healthcare reimbursements.
After providing healthcare services to the patients, the hospital processes the information and sends the claims to the insurance company. While healthcare providers usually get reimbursed by the payer, some of them face expensive hiccups. Due to billing or coding issues, patient identification errors, medical record mix-ups, or other problems, the payer identifies inconsistencies after receiving claims, and they might reject or deny said claims. While some claims can be resubmitted, checking for and fixing the errors is time-consuming, costly, and requires a considerable number of resources.
All of the above leads to back-and-forth exchanges between care providers and payers. Insurers have to reject claims, caregivers lose out on a significant amount of revenue, and many patients even receive shocking, incorrect bills. However, some even lose healthcare services, especially those associated with Medicaid.
Let’s take a look at a few statistics to see how Medicaid patients suffer due to denied medical claims. However, do keep in mind that denied claims can be detrimental for any patient.
A worrying study regarding denied claims
A very recent study has shed light on denied claims and how physicians or hospitals are reluctant to see Medicaid patients due to reimbursement issues.
According to the study, at least 25% of Medicaid claims have been denied upon initial submission. On the other hand, 7.3% of Medicare claims were denied whereas commercial insurers denied 4.8%.
Moreover, the study also states that around 17% of revenue is lost due to billing problems associated with Medicaid patients, whereas the numbers are quite lower for patients covered by Medicare (5%) and other payers (3%).
While any type of denied claim is extremely costly, the statistics show that the Medicaid ones are quite problematic. Moreover, since Medicaid is associated with low-income families, reimbursements are lower as well.
All of this just leads to caregivers being reluctant to look after Medicaid patients.
Denied medical claims are preventable
One of the topmost priorities of physicians and healthcare providers is to look after the patients, Medicare or otherwise. Instead of worrying about denied claims, hospitals and health systems can work on reducing or eliminating them with the right tools and strategies.
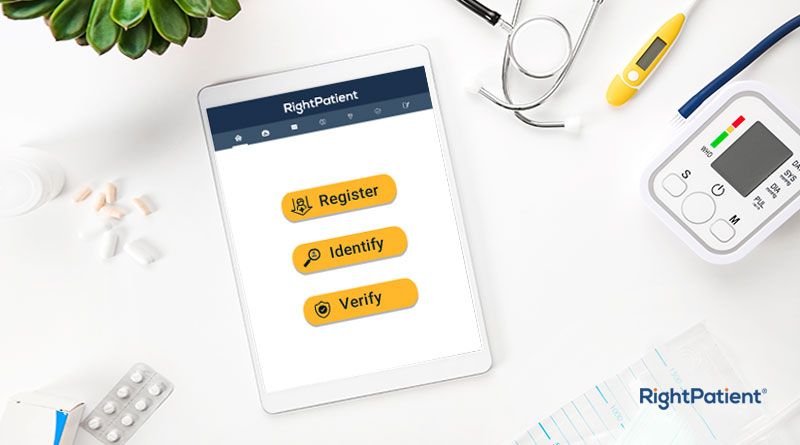
Fortunately, RightPatient, the industry’s leading touchless biometric patient identification platform, can help reduce denied claims substantially.
Denied and rejected claims typically occur because of billing and coding errors – most of which can be traced back to medical record errors, patient mix-ups, and identification issues. RightPatient eliminates all of that, and more, as it ensures that the accurate information is fed to the correct EHR at all times. As a result, billing and coding errors are drastically reduced and so are denied claims – boosting the bottom line.
How are YOU reducing denied claims in your healthcare facility?