To Enjoy Advantages of Telemedicine in Healthcare, Providers Must Protect Patients Online

Telemedicine, many times used interchangeably with the word telehealth, has grown tremendously during last year because of COVID-19. Whilst it’s been available for a long time (decades, really), its future was uncertain before now. Healthcare experts mainly debated about the possible advantages of telemedicine in healthcare, while patients were wary regarding online doctor appointments.
Still, because of COVID-19, practically everything is different, and desperate times required drastic measures. Rules enveloping virtual visits got relaxed, so, more providers and their patients got exposed to this new phenomenon called telehealth.
Online appointments currently have numerous supporters
The user base for telehealth has soared, with numerous healthcare professionals and their patients supporting it and saying they want it to be a permanent part of healthcare after the emergency is over. It was also extremely helpful and convenient throughout the pandemic. That being said, let’s look closer and examine the advantages of telemedicine in healthcare plus the way providers can safeguard their patients throughout these appointments.
A few advantages of telemedicine in healthcare
Telemedicine is cost-efficient for all
The universal understanding regarding virtual healthcare is that it is less expensive than in-person visits. Plus, it saves time, no need to travel to use it, etc. Whilst that’s correct, online healthcare is also less expensive for healthcare providers. Think about it – for most online appointments, all the provider requires is an online platform, the proper devices to connect with their patients, plus a steady, secure online connection. These types of appointments get rid of a lot of the costs linked with traditional healthcare – i.e. registration desks, using paper products, fewer staff members required, etc.
The AHA (American Hospital Association) even agrees with the aforementioned – online healthcare saved over 11% of costs for many hospitals.
Online appointments provide access to many more patients
Even the toughest critics can’t refute the fact that telehealth offers top-notch care to many more patients than in-person appointments. Consider how it worked before COVID-19 – the majority of patients in rural areas were unable to get to a suitable hospital for several reasons.
An example of one of the top advantages of telemedicine in healthcare is that one can use it from any place – so it’s quite convenient for those who live in rural areas. Whilst a tiny amount of providers offered online appointments prior to the pandemic for rural patients, the pandemic showed how helpful telehealth can be for routine patients too. Online appointments assisted in providing top-notch care to a huge number of patients who had various problems – a lot still use this and the experts want it to become a permanent option for healthcare.
Telemedicine fits more people’s needs
Preventive medicine, improved quality, superior scheduling experiences – online appointments can meet all those things and even more!
Numerous experts say because patients are more involved with telehealth appointments than with in-person appointments, the former could encourage more preventive medicine usage. Patients, likewise, feel that they are getting more personalized care with telehealth appointments since they report during in-person appointments that their physicians do not even look at them – only at their computer screens. These cases, along with other factors, might cause a surge of usage that helps to improve healthcare outcomes in the future.
Online appointments offer a superior quality of care for a lot of patients, particularly rural ones, as described earlier. With online appointments, patients can pick which provider they want, and they can even be miles away and still get one that meets their precise healthcare needs.
Finally, with online appointments, patients can merely pick the timeframe that works best for them, so, scheduling is easy. Whilst that also can happen with regular in-person appointments, the patient now doesn’t have to wait hours or longer to see their doctor, all they have to do is log in at their appointment time and see their doctor.
Still, whilst telehealth has a huge possibility, it remains pretty new, so several challenges have to be solved – one is protecting patient information online.
Providers have to safeguard their patients online to enjoy the advantages of telemedicine
Patient records and data are very sensitive information, which is one of the dominant reasons most data breaches occur in the healthcare industry. Hackers can sell a medical record for thousands of dollars on the black market, and the scammers then buy them and use them to get healthcare and the actual patient is charged with the bills. While this normally happens in traditional in-person appointments, a lot of experts believe it can also occur in online appointments, so, the healthcare providers have to safeguard their patients’ information while they are in an online appointment too.
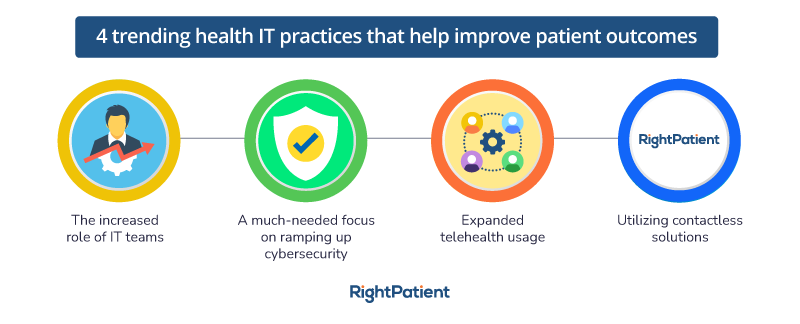
Luckily, RightPatient comes with lots of great experience in protecting patient data as well as avoiding medical identity theft in real-time.
One of the top touchless patient ID platforms utilized by many healthcare providers, RightPatient detects patients via facial recognition and averts scammers from trying to pass as the real patient during the registration process and beyond.
RightPatient can be used during telehealth appointments – so it is perfect for protecting your patient’s information as well as stopping identity theft during virtual visits. Patients only need to take a picture of themselves and a picture ID like their driver’s license – RightPatient takes it from there.
Is your facility ready to safeguard your patients’ info and stop medical identity theft in real-time?